Pelvic Floor Therapy 101
September 11, 2024
Categories: Women's Health
Tags: pelvic pain, bladder problems, cystitis, pelvic floor therapy, pelvic floor exercises
By Jill Howell, physical therapist
Pelvic floor therapy may be new to many patients, but it can make a huge difference in their quality of life. Pelvic floor physical therapy treats: 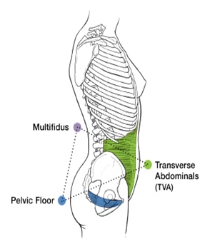
-
Pelvic pain
-
Bladder and bowel dysfunction
-
Pre- and post-partum issues
This illustration shows that the pelvic floor is one-third of the pelvic pyramid. Problems in one area of this pyramid are often associated with problems in another area. Think of this unit as your “floor and core.”
Pelvic floor muscles do not have structures below them for support. So, as with many muscles of the body, these muscles need exercise to keep them functioning properly.
Causes of Pelvic Pain
There are many causes of pelvic pain. The best way to determine the cause is by consulting a medical professional. Causes may include:
-
Interstitial cystitis: chronic pelvic or bladder pain/pressure along with urinary urgency and frequency
-
Dyspareunia: pain before, during, or after intercourse
-
Muscle spasms: muscles tighten and shorten causing pain with movement
-
Labral tears: damage to the cartilage around the hip joint socket
-
Post partum: pain following birth trauma
-
Endometriosis: painful growth of tissues inside the uterus growing outside of the uterus
-
Scar tissue: pelvic pain resulting from trauma to the hip, back, or abdomen
Your Bladder Health Quiz
If you answer yes to any of the following questions, your bladder may be controlling your life, and you may have a problem that could benefit from pelvic floor therapy.
-
Do you urinate more than every two hours in the daytime?
-
Do you urinate more than once (or twice for older patients) after going to bed?
-
Do you have trouble making it to the toilet on time when you have the urge to go?
-
Do you strain to pass urine?
-
Are there times when you are not aware that you needed to use the toilet?
-
Do you empty your bladder frequently, before you experience the urge to pass urine?
-
Do you have the feeling that you are not emptying fully?
-
Do you have a slow or hesitant urine stream?
-
Do you have trouble starting your urine stream?
-
Do you have triggers that make you feel you cannot wait to go (such as running water)?
-
Can you contract your muscles to stop your urine when sitting on the toilet?
-
Do you experience an urge to go but when you get to the toilet, little urine comes out?
Bladder Basics
Normal, healthy bladders can hold up to two cups of water and do not need to be voided for two hours. Typically, an adult will void six to eight times in one 24-hour period, and each time, the stream of urine should be constant and uniform.
Adults with urges to void their bladders too frequently may delay voiding in order to “train” their bladder to send a signal when it is truly full. For more complete voiding, females should sit with both “cheeks” on the toilet seat, and always wipe front to back to avoid hygiene issues that can lead to urinary tract infections.
Certain foods and liquids can irritate the bladder, leading a person to think that voiding is necessary when it may not be. Such irritants include caffeine, citrus fruit, spicy foods, tomato-based products, artificial sweeteners, and milk products.
Constipation
Normal bowel movements look like a sausage, snake, or banana. They are soft and smooth. Very soft, mushy, or liquid stools are called diarrhea. Harder, rigid, and lumpy bowel movements (can be small like nuts or shaped like a sausage) are signs of constipation.
Signs of constipation include straining and a hard stool, a bowel movement less than three times a week, or a feeling that the bowel movement is not complete, yet nothing more comes out.
Constipation is caused by lack of fiber in the diet, hydration, and exercise. Certain medications can also have constipation as a side effect.
Toileting Habits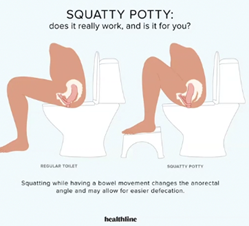
Establishing a bowel routine can be helpful and may take a week or more to become a new habit. This includes eating meals at the same time, not introducing too many new foods, and working toward emptying your bowels at the same time daily.
Use exercise, diet, and colon massage to stimulate a bowel movement. Massage your colon in a clockwise fashion, with your head at 12:00 and your pelvis as 6:00.
Never delay responding to an urge for a bowel movement; do not spend more than 10 minutes trying to have a bowel movement. If you are unproductive, wait and try again later.
Sometimes repositioning on the toilet is helpful. The “Squatty Potty” position may work for you. With this illustration, you can see how a Squatty Potty® changes the angle of the rectum, making it easier to defecate.
Pelvic Floor Evaluation — What to Expect
It is time to look for a pelvic floor therapist if you have leaking, pain, are pre/post-natal with symptoms, or have incomplete emptying or constipation. You will need a referral.
At an appointment you will receive one-on-one care in a private room. You will be asked about your medical history and current triggers. We want to know about your diet, exercise, and bowel habits.
You will also be examined in your low back/core and hip. However, the best way to get a clear picture of the causes of your pain and other symptoms is to do an internal examination that checks your pelvic floor muscles and checks for a prolapse.
Following the examination, treatment options will be presented along with education about your condition.
Treatment Options
The most common treatment options include breathing and relaxation techniques, strengthening of your core back and hips, and strengthening your pelvic floor with and without biofeedback (Kegel exercises). Other treatment techniques include cupping to loosen adhesions, internal stimulation for muscle spasms, and trigger point release using a dilator.
Don’t let pelvic pain or discomfort hold you back any longer. Trinity Health’s experienced team of physical therapists are here to support you on your recovery journey. Take the next step toward better health by contacting your primary care provider or OB/GYN for a referral.




